Researchers at Columbia University have developed a non-invasive technique to permanently correct nearsightedness, a common vision problem already affecting nearly half of the U.S. population.
The study is published in Nature Photonics.
The problem
Although we don’t know what causes it yet, nearsightedness, or myopia, is an increasing problem around the globe. According to the National Eye Institute, 42 percent of Americans ages 12 to 54 are nearsighted. Almost 50 percent of the world’s population will be nearsighted by 2050.
There are two types of solutions currently available to patients: glasses and/or contact lenses and refractive surgeries. However, these solutions are either short-term or invasive with possible side effects. In worst cases, refractive surgeries can lead to permanent vision loss.
While many are searching for less invasive, yet long term alternatives, the Columbia team has developed just that — a non-invasive technique that uses ultrafast lasers to permanently correct vision.
The study
The researchers used a femtosecond oscillator, an ultrafast laser that delivers pulses of very low energy at high repetition rate and can be used to cut very thin glasses.
“During my doctoral work I was interested in interaction between glass and femtosecond lasers. Cornea, just like glass, is a transparent dielectric, and hence the connection,” said Sinisa Vukelic, a lecturer in the Department of Mechanical Engineering and the lead researcher. “I thought that must be more that we can do with the femtosecond lasers than to cut.”
Vukelic was right. This technique allows for just enough power to induce a low-density plasma within the set focal volume that causes ionization of water molecules within the cornea, but doesn’t cause damage to the tissue within the treatment region.
This ionization creates a reactive oxygen species, a type of unstable molecule that contains oxygen and that easily reacts with other molecules in a cell, which in turn interacts with the collagen fibrils to form chemical bonds, or crosslinks. The selective introduction of these crosslinks induces changes in the mechanical properties of the treated corneal tissue.
“We’ve seen low-density plasma in multi-photo imaging where it’s been considered an undesired side-effect,” Vukelic said in a statement. “We were able to transform this side-effect into a viable treatment for enhancing the mechanical properties of collagenous tissues.”
Their method alters biochemical and biomechanical properties of collagenous tissue without causing cellular damage and tissue disruption. Unlike refractive surgeries, this technique doesn’t involve a surgery and has fewer side effects and limitations.
“We think our study is the first to use this laser output regimen for noninvasive change of corneal curvature or treatment of other clinical problems,” Vukelic said in a statement.
The results
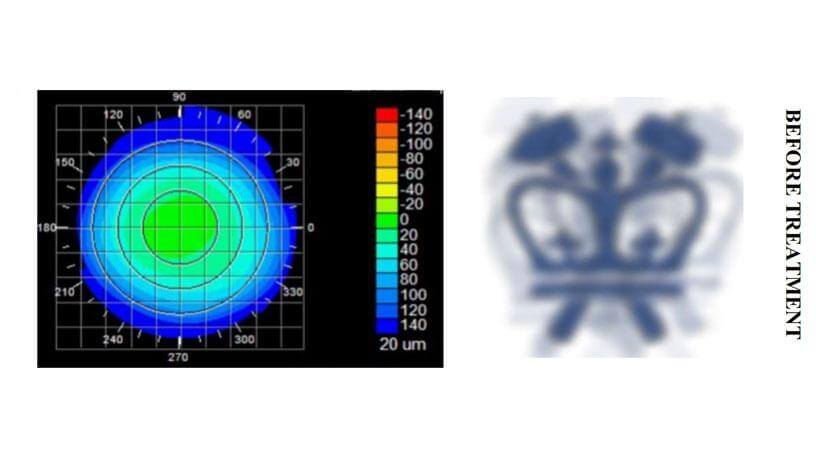
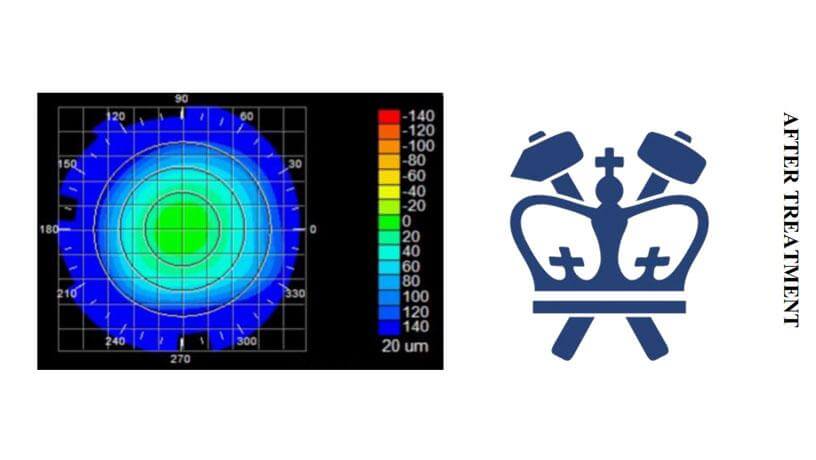
When this technique is applied to corneal tissue, the crosslinking alters the collagen properties in the treated regions. Ultimately, this results in changes in the overall macrostructure of the cornea.
While avoiding optical breakdown of the corneal tissue, the treatment ionizes the target molecules within the cornea. Because the process is photochemical, it does not disrupt tissue and the induced changes remain stable.
“If we carefully tailor these changes, we can adjust the corneal curvature and thus change the refractive power of the eye,” Vukelic said in a statement. “This is a fundamental departure from the mainstream ultrafast laser treatment that is currently applied in both research and clinical settings and relies on the optical breakdown of the target materials and subsequent cavitation bubble formation.”
The next step
The researchers are looking to develop a way to predict corneal behavior as a function of laser irradiation. If they knew, for example, how the cornea might deform if a small circle or an ellipse were treated, they will be able to personalize the treatment — they could scan a patient’s cornea and then use the team’s algorithm to make patient-specific changes to improve his/her vision.
They are also in the early stages of building a clinical prototype and planning to start clinical trials by the end of the year.
“At this moment we are mostly discussing with various experts on how to proceed, while simultaneously working on the clinical prototype,” said Vukelic. “We are now balancing enthusiasm with the caution to ensure everything is done properly.”