Breast cancer is among the leading causes of death in the U.S.
According to the National Cancer Institute, roughly 268,670 new cases of breast cancer are expected this year, and 40,920 women are expected to die from the disease.
Additionally, one in eight women will develop breast cancer at some point in their lives.
Unfortunately, more than 50 percent of mammograms in the U.S. are flawed.
Whether it be failure to provide a correct image or misinterpretation by a doctor, inaccurate mammograms often lead to costly misdiagnoses or failure to catch a deadly tumor.
Scientists are therefore looking to AI to provide patients with more accurate mammogram results.
Mammograms are flawed
Doctors can fail to accurately detect a tumor from the reading, which can result in a false-negative test.
Oppositely, doctors might misinterpret the screening as positive even when it’s not, which can result in a false-positive test and require the patient to go through additional unnecessary and expensive testing.
“Mammograms can be a valuable and life-saving screening for breast cancer in certain cases,” said Morgan Statt, a health and safety investigator at ConsumerSafety.org.
“But there are a number of flaws that exist within mammography that should encourage us to continue to improve the tests. From a purely economic standpoint, false-positive mammogram results equate to $4 billion in national spending each year due to additional testing and invasive procedures.”
Furthermore, current mammograms are unable to detect fast-developing interval cancers between screenings.
Taken as a whole, each of these issues can be detrimental to both the physical and emotional health of a patient.
“Coupled with the financial impact of flawed mammogram testing is the emotional turmoil experienced by the patient,” said Statt.
“Psychological distress and anxiety can be experienced by women who have received false-positive results, while false-negative screenings can bring up short-lived moments of hope. These two reasons alone should encourage the continuous improvement of mammogram results.”
How AI can help
AI can be used to improve the accuracy of mammograms by eliminating human error and increasing the speed of mammography readings.
Since inaccurate readings are often the result of a misinterpretation by the doctor, scientists have begun using both machine learning and deep learning, a subset of AI, to improve accuracy.
“So far, the application of AI in mammography has shown that it can improve the accuracy of the screenings, help doctors diagnose at much faster rates, and can even improve workflow efficiencies within radiology on a per-facility basis,” said Statt.
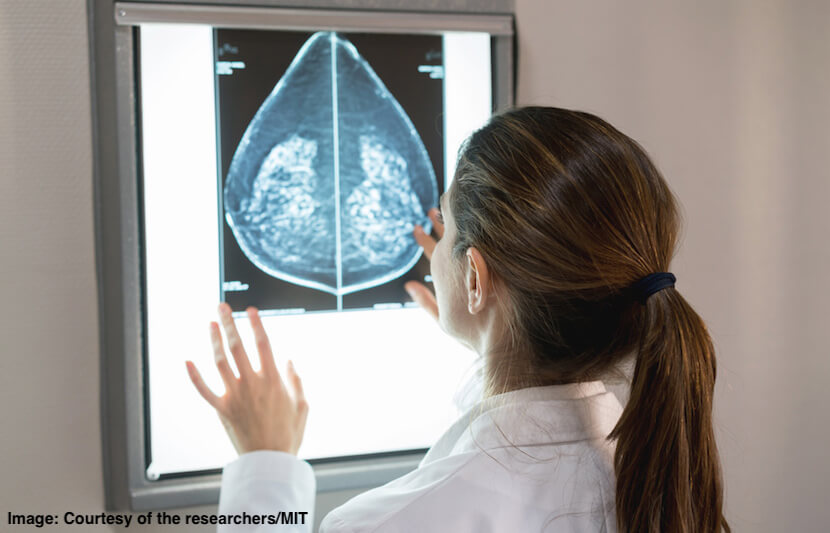
Assessing dense tissue
In a recent study, MIT and Massachusetts General Hospital researchers demonstrated that their deep-learning model can be used to assess dense breast tissue as accurately as human experts.
Dense breast tissue is a risk factor for breast cancer, which is why doctors in 30 U.S. states are required by law to inform patients whose mammograms identify dense tissue.
However, while over 40 percent of women in the U.S. have dense breast tissue, breast density assessments can vary for a variety of reasons.
“Breast density is an independent risk factor that drives how we communicate with women about their cancer risk,” Adam Yala, a doctoral student in MIT’s Computer Science and Artificial Intelligence Laboratory (CSAIL) and second author of the study, said in a statement.
“Our motivation was to create an accurate and consistent tool, that can be shared and used across health care systems.”
In both training and testing, the model learned to identify four categories of breast density — fatty, scattered, heterogeneous and dense — from expert radiologists.
The model proved to be as reliable as human experts. The researchers found, for example, that the model matched MGH radiologists’ assessments on more than 10,000 mammograms at 94 percent.
The researchers plan on scaling their model so they can make it available to other hospitals
Distinguishing malignant and benign diagnoses
In another recent study, researchers from the University of Pittsburgh found that their deep-learning technology could help doctors identify nuanced mammographic imaging features on false-positive tests that can help them distinguish between malignant and benign diagnoses.
The scientists were able to identify unique and hard-to-read imaging features that can help radiologists assess whether a reading is truly positive or negative.
“AI, particularly the deep learning techniques, provide a data-driven approach to identify potential imaging features that may be hard to be visually assessed/perceived by radiologists in reading the images,” said Shandong Wu, an assistant professor of radiology, biomedical informatics and bioengineering at the University of Pittsburgh.
“Thus, with AI and a large set of screening mammogram images, it provides an important scheme to help solve the issue.”
Interpreting mammograms
Scientists at the Houston Methodist Research Institute have developed an AI program that can interpret mammograms with 99 percent accuracy and 30 times faster than a human doctor.
The team used AI software to evaluate mammograms and pathology reports of 500 patients. The software was programmed to scan patient charts, collect diagnostic features and correlate mammogram findings with a breast cancer subtype.
It took just a few hours for the program to complete all 500 patient readings. A manual review of just 50 charts would typically take two clinicians 50-70 hours to complete.
The scientists then used the results to accurately predict each patient’s probability of breast cancer diagnosis.
Conclusion
The development of AI for more accurate mammograms is crucial to women’s health around the world.
“I think AI applications of mammogram testing should continue to develop to help radiologists better interpret these scans, if only to propel forward our continued interaction with computer systems,” said Statt.