A revolutionary MRI scan method, developed by Newcastle University, offers unprecedented real-time insights into lung function, aiding the diagnosis and treatment of respiratory diseases and lung transplant monitoring.
In a breakthrough that could transform respiratory health care, scientists at Newcastle University in the UK have devised a novel lung scanning technique that reveals a real-time view of lung function.
This pioneering method, leveraging the harmless gas perfluoropropane, enables clinicians to see how air moves through the lungs of patients with conditions such as asthma, chronic obstructive pulmonary disease (COPD) and those who have undergone lung transplants.
The research team conducted two studies that detailed the use of this specialized gas. When patients inhale and exhale the gas during an MRI scan, the technology shows precisely where in the lungs the gas has traveled, offering a clear picture of lung ventilation.
Pete Thelwall, a professor of magnetic resonance physics and director of the Centre for In Vivo Imaging at Newcastle University who led the research, highlighted the significance of the scans.
“Our scans show where there is patchy ventilation in patients with lung disease, and show us which parts of the lung improve with treatment,” he said in a news release. “For example, when we scan a patient as they use their asthma medication, we can see how much of their lungs and which parts of their lung are better able to move air in and out with each breath.”
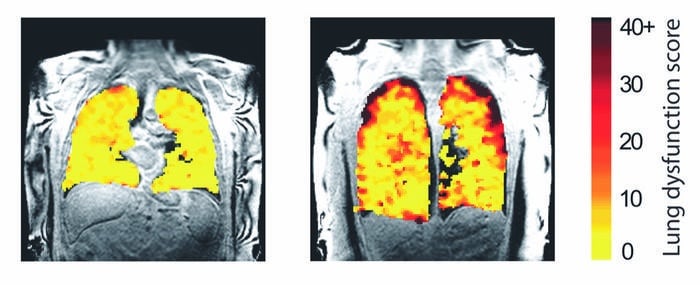
Caption: Lung function MRI showing problem areas (measurement levels of dysfunction) in lung transplant recipients.
Credit: Newcastle University, UK
This advancement lets medical professionals evaluate the severity of respiratory diseases by measuring well-ventilated and poorly ventilated lung areas. The first study, published in the journal Radiology, underscores the potential of the new scanning technique in clinical trials for asthma and COPD treatments.
The researchers have been able to use this method to quantify improvements in lung ventilation following the administration of common bronchodilators like salbutamol.
In another significant study published in the journal JHLT Open, the team applied this method to lung transplant recipients. By tracking the movement of air in the transplanted lungs, they could identify early signs of chronic lung allograft dysfunction — a common and serious complication where the immune system attacks the transplanted lung tissue.
“We hope this new type of scan might allow us to see changes in the transplant lungs earlier and before signs of damage are present in the usual blowing tests,” added co-author Andrew Fisher, a professor of respiratory transplant medicine at Newcastle Hospitals NHS Foundation Trust and Newcastle University. “This would allow any treatment to be started earlier and help protect the transplanted lungs from further damage.”
This innovative scanning technique holds promise for the future of lung disease management. It brings a heightened sensitivity to detecting changes in lung function, paving the path for earlier interventions and better patient outcomes.

